Clinical Resources
Here you will find a broad range of information on different treatments and diagnoses.
We have organized this information by conventional discipline. If you aren't finding the information you are looking for, please contact us.
Parasympathetic and Sympathetic (P&S) Monitoring helps to maintain wellness and prevent dysfunction, disorder, or disease.
When possible, lifestyle changes and supplements are employed to help maintained wellness. Whether pharmaceutical therapy is prescribed or not, wellness is promoted by maintaining a proper balance and coordination between the P&S nervous systems.
This is because of 2 factors:
1) All organs and organ systems are controlled or coordinated by the parasympathetic and sympathetic (P&S) systems, and
2) It is the purpose of the parasympathetic and sympathetic (P&S) systems to maintain normal organ function even when the P&S systems themselves are out of balance, then parasympathetic and sympathetic (P&S) dysfunction precedes organ dysfunction and symptoms are not demonstrated until the organs become dysfunctional.
Normalizing P&S imbalance before symptoms, prevents symptoms, and maintains wellness.
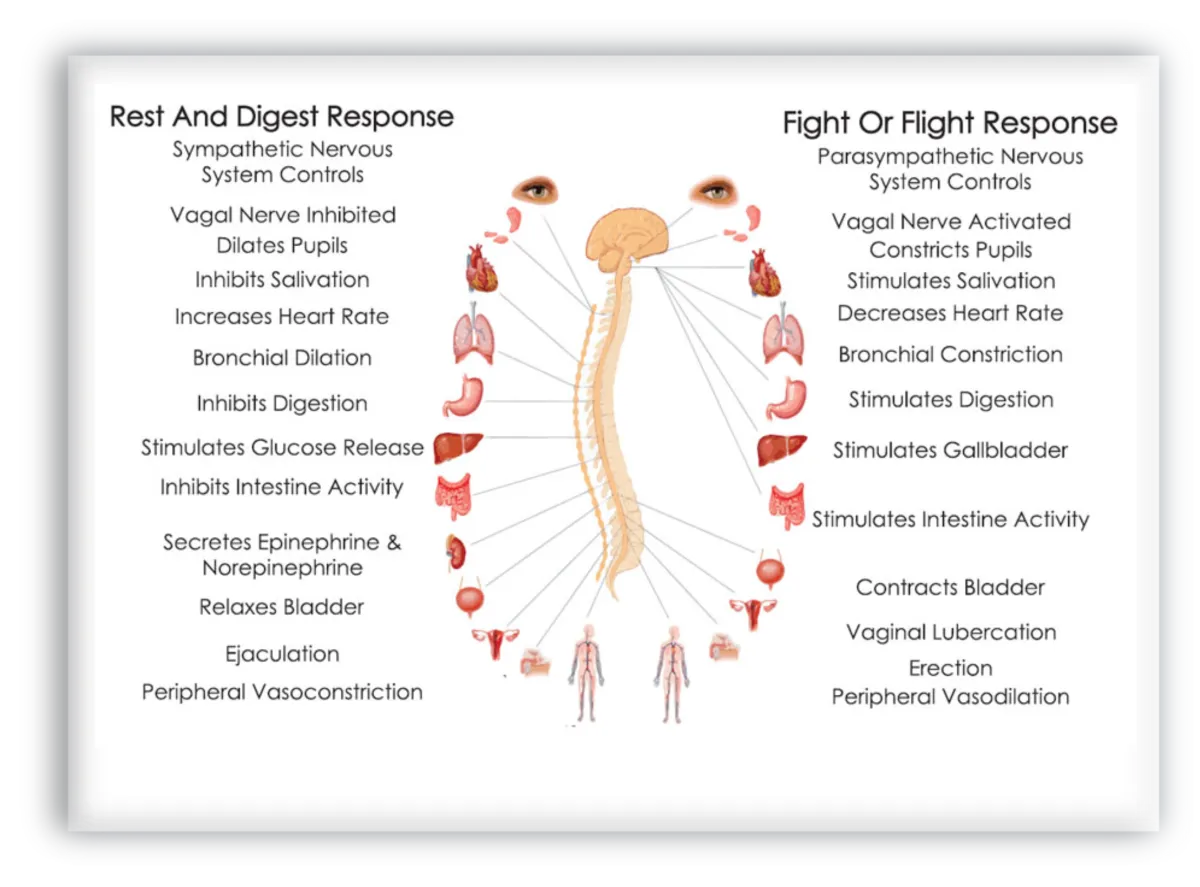
It’s divided into two primary branches:
Sympathetic Nervous System (SNS)
Often referred to as the "fight or flight" system, it prepares your body to respond to stress or danger by increasing heart rate, dilating airways, and redirecting blood flow to muscles.
Parasympathetic Nervous System (PNS)
Known as the "rest and digest" system, it slows the heart rate, promotes digestion, and supports recovery and repair.
The balance between these two branches is critical for health, resilience, and healing.
Physio PS provides unprecedented insight into the physiological responses of the autonomic nervous system.
In general, Parasympathetic and Sympathetic (P&S) Monitoring helps to diagnose and treat patients, enhancing the ability to return health and establish wellness. Once wellness is established (or if the patient was well to begin with), Parasympathetic and Sympathetic (P&S) Monitoring helps to maintain wellness and prevent dysfunction, disorder, and disease.
How Can We Monitor the Autonomic Nervous System?
Thanks to advances in technology, we can now assess the health of the autonomic nervous system using non-invasive tools like Physio PS, a system deployed worldwide and utilized by physicians, clinicians, and researchers.
Physio PS can provide real-time data on how the body’s nervous system responds to stress, movement, and recovery. This data can guide healthcare providers — including, general physicians, cardiologists, neurologist, osteopaths, endocrinologists, physical therapists, chiropractors, and more — to make more informed treatment decisions, especially for patients who aren’t improving with standard care.
Parasympathetic and Sympathetic (P&S) Monitoring Helps to Treat.
With the additional information from P&S Monitoring, more specific and individualized therapy plans may be developed. Some diagnoses maybe either parasympathetically-mediated or sympathetically mediated, yet both mediations lead to the same set of symptoms.
For example, hypertension may be a primary, Sympathetic excess, or may be a Sympathetic excess (SE) secondary to a (primary, co-existing) Parasympathetic excess (PE); both autonomic branches are over-active.
If hypertension is due to a primary SE, standard sympatholytics (e.g., antihypertensives) is indicated.
If hypertension is due to a SE secondary to PE, therapy should first treat the PE, and then if any SE remains, complete the therapy plan with sympatholytics.
Note, this tends to be the more difficult to manage form of hypertension.To treat PE without co-morbid heart disease, consider low-dose anticholinergic therapy (in the form of very, low-dose antidepressant).
If hypertension is due to a SE secondary to PE, therapy should first treat the PE, and then if any SE remains, complete the therapy plan with sympatholytics. Note, this tends to be the more difficult to manage form of hypertension.
Parasympathetic and Sympathetic (P&S) Monitoring Helps to Diagnose.
Most chronic diseases involve at least one of 4 autonomic dysfunctions. Classified as high or low Parasympathetic (P), or high or low sympathetic (S); at rest or when challenged. Restoring or establishing P&S balance (i.e., normalizing Sympathovagal Balance (SB) at rest, or returning proper coordination upon challenge) reduces the individual’s morbidity and mortality risk, as well as the number of co-morbidities. Once the P&S nervous systems are properly balanced, both at rest and coordinated upon challenge, any remaining symptoms are due to end-organ effects. These symptoms may now be more aggressively treated.
Physio PS specializes in the development of custom software solutions helping healthcare organizations to predict risk of chronic disease and catastrophic injury by leveraging the Medicare Annual Wellness Visit.
Physio PS provides physicians with a custom complete solution for processing the Medicare Annual Wellness Visit (AWV) for your Medicare Part B and Medicare Advantage patients.
Physio PS is committed to provide healthcare professionals with the opportunity to enhance patient care while contemporaneously increasing practice revenue.
Physio PS Services is designed to operate as the preeminent leader in comprehensive and technologically advanced medical solutions for healthcare professionals across the nation, by providing state-of-the-art, medical technology and services affording their patients transcending preventative care, while increasing practice revenue potential.
At Physio PS, improving healthcare is our focus and passion. Our custom client platform provides the finest technology based on advanced scientific principles, complemented by medical technology support services.
Recognizing technology and medical science is rapidly evolving, ANS monitoring with Physio PS enables our physicians with an innovative approach to address health and wellness challenges across the broad spectrum of healthcare disciplines.
NEUROLOGY
Headaches
There are numerous reasons for headaches: medication mismanagement, neurologic, cardiologic, etc. P&S Monitoring provides more information to further differentiate. Whether P or S, P&S-mediated headaches are associated with improper brain perfusion (too little or too much, respectively), triggering the neurological effects that underlie headache. P&S Monitoring specifies which and enables more specific therapy. Once P&S balance is established, any remaining symptoms are due to a brain disorder.
Tension Headache
There are numerous reasons for tension headaches. Tension tends to indicate high SB or challenge SE.
Migraine
Like headache, there are many forms of migraine, some Parasympathetically-mediated alike headaches, there are many forms of migraine, some Parasympathetically-mediated and some Sympathetically mediated. Whether P or S, P&S-mediated migraines are associated with improper brain perfusion (too little or too much, respectively), triggering the neurological effects that underlie migraine. P&S Monitoring specifies which and enables more specific therapy. Once P&S balance is established, any remaining symptoms are due to a brain disorder.
ADD/ADHD
ADD/ADHD is characterized by a dynamic (challenge) PE that causes a challenge SE that is responsible for both the attention deficit and the hyperactivity. In essence, the PE induces a form of depression due to PE-induced marginal or poor brain perfusion. The secondary SE causes the “adrenaline storm” that underlies the attention deficit and the hyperactivity. We have had success switching these patients from the standard therapies (characterized by high dose, long-term) to low-dose, short-term anti-cholinergic therapy, and have relieved the disorder within 18 months. Once P&S balance is established, any remaining symptoms are due to a brain disorder.
Parkinsonism, Parkinson’s Disease
As a catecholaminergic disorder, the P&S nervous systems are involved. While P&S balance helps to maintain quality of life longer, it does not always help to slow the disease process. P&S Monitoring will identify autonomic neuropathy, including Cardiovascular Autonomic Neuropathy, to help minimize mortality risk.
Depression
Depression is characterized by PE, either resting or challenge, or both. All antidepressants are types of anti-cholinergics. The less the BP effect of these medications, the less of a P&S effect. Depression that persists after P&S are balanced, is psychological. P&S imbalance is the physiologic component and is associated marginal or poor brain perfusion. Once P&S balance is established, any remaining symptoms are psychological issues.
Bipolar Disease
From a P&S perspective, Bipolar Disease is a primary PE disorder; therefore, and primary depression disorder. Once the PE is normalized, the SE (secondary to PE) is typically relieved organically, without additional medication. With P&S imbalance, the anxiety phases of Bipolar Disease are cycled when brain perfusion becomes too low, typically after an event that is associated with increased Parasympathetic tone (after large meals, before bedtime, after emotional responses). Once P&S balance is established, any remaining symptoms are psychological issues.
Anxiety
There are two underlying P&S forms: (1) resting high SB (indicating resting SE) as the primary P&S disorder; and (2) challenge PE, causing secondary SE, releasing excess adrenaline causing anxiety secondary to the challenge PE. The latter involves depression. The commonly experienced heart palpitations, in either case, are due to the associated SE, but are typically not life threatening due to SE that is not critical. Once P&S balance is established, any remaining symptoms are psychological issues.
Post-Traumatic Stress Disorder (PTSD)
PTSD is associated with what are known as “Quality of Life” (QoL) symptoms: sleep, GI, bladder and bowel dysfunction, lightheadedness upon standing, sex dysfunction, high BP, and depression. The opposing symptoms of depression and high BP help to confirm that PTSD involves both PE and SE; specifically challenge PE, leaving the SE as secondary. While P&S monitoring and guided therapy help to normalize QoL symptoms, it does not directly address the “trigger;” however, it has been found that once the QoL symptoms are normalized, patients are significantly better able to manage the trigger.
Sleep Disorders
Disorders characterized by night-time sleeplessness are associated with SE, and disorders characterized by day-time sleepiness are associated with PE. Once P&S balance is established, any remaining symptoms may be psychological, hormonal, or neurological issues.
Shy-Drager Syndrome (Orthostatic Hypotension with Multisystem Degeneration, aka Multiple System Atrophy (MSA))
MSA and Parkinson’s Disease are nearly identical in the early stages. Treating one with the therapy for the other, accelerates the progression of the one. Since Parkinson’s Disease preserves Sympathetic innervation to the heart, P&S Monitoring differentiates the two earlier, helping to ensure proper therapy planning. Once P&S balance is established, any remaining symptoms are due to the disorder itself.
Idiopathic Peripheral Autonomic Neuropathy
Idiopathic Peripheral Autonomic Neuropathy is one of the earliest signs of P&S dysfunction, enabling earlier and more aggressive therapy to slow or stay the progression of autonomic neuropathy by establishing and maintaining P&S balance.
Chronic Regional Pain Syndrome (CR or Reflex Sympathetic Dystrophy (RSD)
CRPS is characterized by pain with both SE and PE. The SE due to the “stress” of pain and the PE due to compromised blood flow (e.g., due to plexus damage) to one or multiple regions of the body.
Multiple Sclerosis
While P&S balance helps to maintain quality of life longer, it does not always help to slow the disease process. P&S Monitoring will identify autonomic neuropathy, including Cardiovascular Autonomic Neuropathy, to help minimize mortality risk.
Polyneuropathy: Diabetic, Idiopathic, or other
Sensory and motor neuropathies are preceded by autonomic neuropathy causing poor circulation inducing or exacerbating the others.
Myasthenic Syndrome (Eaton-Lambert)
This disease also affects the P&S systems. While P&S balance helps to maintain quality of life longer, it does not always help to slow the disease process. P&S Monitoring will identify autonomic neuropathy, including Cardiovascular Autonomic Neuropathy, to help minimize mortality risk.
Orthostatic Hypotension
In general, Orthostatic dysfunction is associated with alpha-sympathetic (adrenergic) insufficiency (Sympathetic Withdrawal, or SW) causing lower extremity vascular dysfunction upon standing, which causes a drop in BP upon standing (head-up postural change). P&S Monitoring quantitatively specifies SW, helping to differentiate Orthostatic dysfunction, including Orthostatic Intolerance, Orthostatic Hypotension, Orthostatic Hypertension, and Postural Orthostatic Tachycardia Syndrome (POTS), from other causes of dizziness and lightheadedness (including Syncope). Treat the SW to relieve any of the forms of Orthostatic dysfunction. Note, the majority of patients with Orthostatic dysfunction are found to simply be dehydrated. Consider proper daily hydration as the primary recommendation.
Syncope and Collapse
In general, Syncope is (beta-) SE with standing (head-up postural change), in other words, a cardiac issue. P&S Monitoring can positively identify Vasovagal Syncope (stand SE with PE), and Neurogenic Syncope (stand SE with an abnormal HR response to stand). Cardiogenic Syncope is a diagnosis by omission. While Neurocardiogenic Syncope is the most commonly diagnosed form, P&S Monitoring helps differentiate the �?neuro’ component from the �?cardio’. Treat PE for Vasovagal syncope. Treat the HR abnormality for Neurogenic. Consider additional cardiac testing, including tilt table, to positively diagnose and treat Cardiogenic Syncope.
Tachycardia (Postural, POTS)
POTS and Vasovagal Syncope are difficult to differentiate, even with tilt-table. P&S Monitoring quantitates the Sympathetic response to stand (head-up, postural change), differentiating stand SW (indicating orthostatic dysfunction, including POTS) from stand SE (indicating Syncope). This is more information that enables more individualized therapy planning, including the possibility of both Orthostatic dysfunction and Syncope concurrently.
Chronic Hypotension
Chronic Hypotension is characterized by low SB or challenge PE. Once P&S balance is established, any remaining symptoms are cardiovascular issues.
Dizziness, Lightheadedness and Vertigo
As indicated above there are multiple reasons for lightheadedness and dizziness, including Vestibular dysfunction, especially in geriatrics. Consider both Vestibular testing and P&S Monitoring to fully document and diagnose and determine therapy.
Chronic Fatigue Syndrome
Chronic Fatigue Syndrome is characterized by low SB or challenge PE.
PULMONOLOGY
Sleep Disturbances (e.g., Central or Obstructive Sleep Apnea)
Sleep Disturbances are characterized by Parasympathetic insufficiency followed by SE. Parasympathetic insufficiency underlies the collapse of the soft palate, and then the stress of not breathing while sleeping and then not sleeping causes the SE. Note, sleep apnea therapies (e.g., CPAP) are not direct sympatholytics; therefore, they only relieve the “stress” of not sleeping. They are not sufficient to reduce the SE associated with typical co-morbidities associated with sleep apnea: hypertension, diabetes, obesity, etc. Additional Sympathetic therapies are needed to normalize the mortality and morbidity risk of sleep apnea. P&S Monitoring is often necessary to properly titrate the additional sympatholytic therapy.
Asthma
Is it a bronchial issue and therefore a Sympathetic dysfunction? The non-steroidal therapies may involve beta-2 adrenergic agonists to broncho-dilate. However, beta-2 adrenergic agonists also affect the heart, increasing HR or BP by causing SE. The associated SE that may be induced, precedes the increase in HR or BP, and P&S Monitoring helps to titrate the asthma therapy to manage the disease without inducing heart diseases via the induced SE. Once P&S balance is established, any remaining symptoms may be pulmonary.
COPD (Asthma with Chronic Obstruction)
The non-steroidal COPD therapies may involve beta-2 adrenergic agonists to broncho-dilate. However, beta-2 adrenergic agonists also affect the heart, increasing HR or BP by causing SE. The associated SE that may be induced, precedes the increase in HR or BP, and P&S Monitoring helps to titrate the COPD therapy to manage the disease without inducing heart diseases via the induced SE. Once P&S balance is established, any remaining symptoms may be pulmonary.
CARDIOLOGY
Hypertension
BP is controlled by Baroreceptor Reflex (BRR), which is controlled by the Sympathetics. Hypertension is typically characterized by SE driving up BRR and then BP. At first, hypertension is due to both an initial decline in resting Parasympathetic activity causing high SB (indicating resting SE) and a (protective) challenge PE causing a secondary challenge SE, then it is due to the continuing effects of SE.
Post-MI
MI causes SE; therefore, post-MI symptoms are due to SE.
Angina
The vasculature is uniquely controlled by the Sympathetic nervous system: peripheral vasoconstriction is a function of increased Sympathetic tone increasing BP and shunting blood to the core; peripheral vasodilation is a function of decreased Sympathetic tone decreasing BP and enabling blood flow to the periphery. Angina is a form of Coronary Artery Disease (CAD) and is a function of SE, either due to excess vasoconstriction or due to blockages from atherosclerotic build up.
Atherosclerosis
Atherosclerosis induces SE. It may be induced by SE as SE may involve endothelial dysfunction.
Mitral Valve Prolapse Syndrome
Mitral Valve Prolapse Syndrome is empirically associated with PE, if not a structural cardiac issue.
Cardiomyopathy
Cardiomyopathy is characterized by SE, however, its different forms may be induced by other disorders. For example, Hypertrophic Cardiomyopathy is genetically facilitated, with the disorder turning symptomatic if and when Orthostatic dysfunction (associated with α-SW upon standing) or Syncope (associated with α-SE upon standing) is demonstrated.
Cardiac Dysrhythmias
Cardiac Dysrhythmias are varied and, in part, associated with P&S dysfunction. It is accepted that approximately 80% of atrial dysrhythmias also involve the P&S systems (only 20% are purely cardiogenic). Of the 80% that involve the P&S, approximately 20% are Sympathetically-mediated and 80% are Parasympathetically-mediated. Ventricular dysrhythmias are accepted to also involve the Sympathetics, except repolarizing ventricular dysrhythmias, which are accepted to also involve the Parasympathetics. P&S monitoring helps to specify which branch is involved. Once P&S balance is restored, the remaining symptoms are cardiogenic
Congestive Heart Failure
CHF is characterized by high SB, indicating a resting SE. Note, resting SE (high SB) precedes even the 3% weight gain indicator and which may be prevented with early intervention, including a temporary increase in diuretic, if the increase in SB is noted (up to 4 days) before the weight gain. This helps to avoid hospitalization.
ENDOCRINOLOGY
Thyroid Disorders
The P&S systems are intimately associated with the hormonal systems. Hyperthyroidism is characterized by SE (at least in part) causing the over-production of thyroid hormones. Hypothyroidism is characterized by PE (at least in part) shutting down the production of thyroid hormones.
(Premature) Menopausal Symptoms or Syndromes
The P&S systems are intimately associated with the hormonal systems. From a P&S perspective, menopausal abnormality is characterized by challenge PE, (at least in part) shutting down the production of estrogen and progesterone. Once P&S balance is established, any remaining symptoms are end-organ issues.
Diabetes
By the time of diagnosis, both forms of Diabetes (types I & II) are characterized by SE: (1) at first due to both an initial decline in resting Parasympathetic activity causing high SB (indicating resting SE) and a (protective) challenge PE causing a secondary challenge SE, (2) then due to the continuing effects of sugar acidosis on the more highly exposed Vagus Nerve which comprises the majority of the Parasympathetic Nervous System. In type II Diabetes, Prediabetes is characterized by challenge PE shutting down (at least in part) the production of insulin. Once P&S balance is established, any remaining symptoms are end-organ issues.
NEPHROLOGY
Hypertensive Renal Disease or Renal Failure
Both are typically characterized by SE: (1) at first due to both an initial decline in resting Parasympathetic activity causing high SB (indicating resting SE) and a (protective) challenge PE causing a secondary challenge SE, (2) then due to the continuing effects of uremia toxicity on the more highly exposed Vagus Nerve which comprises the majority of the Parasympathetic Nervous System. In Hypertensive Renal Disease, resting SE is exacerbated either causing, or caused by, the hypertension.
INTERNAL MEDICINE
Morbid Obesity
There are two underlying P&S forms: (1) stress induced, challenge PE (as a protective mechanism), causing secondary SE, releasing cortisol, putting the body into “starvation mode;” and (2) resting low SB (indicating resting PE) keeping metabolism low. Both may involve depression. The former is typically the difficult-to-manage type. The latter is the type that best responds to typical diet programs and is easier to keep off the weight.
Unspecified Immunity Deficiency
The Parasympathetic nervous system provides the immune system its memory and helps to control and coordinate immune responses. Weak P-Activity (including high SB, at rest) promotes immune deficiency.
GERD
The gastric system is uniquely controlled by the Parasympathetics. GERD as a result of PE is due to overactive gastric motility. GERD as a result of Parasympathetic insufficiency is due to forms of gastroparesis. Once P&S balance is established, any remaining symptoms may be specifically gastric (end-organ) issues (e.g., smooth muscle, excess gastric secretion, bacterial, etc.).
Gastroparesis
The gastric system is uniquely controlled by the Parasympathetics. Gastroparesis is (at least in part) a result of Parasympathetic insufficiency. Once P&S balance is established, any remaining symptoms may be specifically gastric (end-organ) issues (e.g., smooth muscle, excess gastric secretion, bacterial, etc.).
Irritable Bowel Syndrome
The intestinal system is uniquely controlled by the Parasympathetics. IBS with constipation is (at least in part) a result of Parasympathetic insufficiency, causing low motility. IBS with diarrhea is (at least in part) a result of PE, causing excess motility. Once P&S balance is established, any remaining symptoms may be specifically gastric (end-organ) issues (e.g., smooth muscle, excess gastric secretion, bacterial, etc.).
Fibromyalgia
Fibromyalgia is now accepted as an autonomic dysfunction, typically characterized by challenge PE. The associated SE (associated with the amplified pain responses) is typically secondary to the PE and is the main reason why it is difficult to control or respond, seemingly paradoxically, to anti-cholinergic therapy.
Edema
Lower body edema is typically associated with SW, causing pooling of blood in the lower vasculature and may result in varicose or spider veins; more generalized edema is associated with PE.
Sex Dysfunction
Sex function requires proper coordination between the P&S systems: P for “point”, responsible for erection and vaginal lubrication, and S for “shoot”, responsible for ejaculation and orgasm. Once P&S balance is established, any remaining symptoms may be vascular, psychologic, or hormonal.
Provider Benefits:
Continuous monitoring of the patient’s current health status using autonomic biomarkers
Evaluation of treatment efficacy and validation of therapeutic interventions
Comprehensive screening for Cardiac Autonomic Neuropathy (CAN) and Diabetic Autonomic Neuropathy (DAN)
Assessment of key cardiovascular and metabolic indicators, including Metabolic Syndrome, Hypertension, and Heart Failure
Early detection of psychological and stress-related conditions such as burnout, anxiety, and depression
Investigation of autonomic involvement in chronic conditions like Asthma, COPD, Palpitations, Pain syndromes, and Sleep Apnea
Personalized optimization of therapeutic strategies based on individual autonomic profiles
Instant generation of detailed reports featuring qualitative, quantitative, and graphical analysis of ANS balance, cardiovascular function, stress response, physical fitness, and overall health
Integration of real-time data with patient medical history to support clinical decision-making and procedural planning
Streamlined, patient-centered management of complex, multi-symptom presentations
Patient Benefits:
Comprehensive evaluation of current health status, including symptomatology, pharmacological response, and therapeutic impact
Analysis of recovery trajectory to determine the appropriateness and effectiveness of ongoing rehabilitation or treatment
Clinical prioritization to address early indicators of chronic disease development or worsening of existing conditions
Prognostic assessment and evaluation of treatment efficacy to guide long-term care planning
Detection of physiological abnormalities within the cardiovascular and cerebrovascular systems, contributing to a holistic health assessment
Vascular health analysis, including arterial elasticity, peripheral circulation efficiency, and identification of organic or functional vascular impairments
Predictive insight into the development and progression of Arteriosclerosis, Obesity, Hypertension, Hyperlipidemia, and Diabetes
Serves as a reliable physiological health indicator—acting as an internal "health barometer" for preventive and diagnostic purposes
Additional Information
Physio PS specializes in the development of custom software solutions to help healthcare organizations to predict the risk of chronic disease and catastrophic injury by leveraging the Medicare Annual Wellness Visit.
Physio PS provides physicians with a complete, custom solution for processing the Medicare Annual Wellness Visit (AWV) for your Medicare Part B and Medicare Advantage patients.
Physio PS is committed to providing healthcare professionals with the opportunity to enhance patient care while at the same time increasing practice revenue.
Physio PS is designed to operate as the preeminent leader in comprehensive and technologically advanced medical solutions for healthcare professionals across the nation by providing state-of-the-art medical technology and services, affording their patients exceptional preventative care while increasing practice revenue potential.
At Physio PS, improving healthcare is our focus and passion. Our custom client platform provides the finest technology based on advanced scientific principles complemented by medical technology support services.

Testimonials
Sean O. Flannagan, PT, DPT, Cert. SMT, Cert. DN, MAACP
"Physio PS has been a gamechanger in uncovering the hidden autonomic dysfunctions that often underlie chronic fatigue, persistent pain, anxiety symptoms, and delayed recovery after whiplash and concussion. It’s given us answers when nothing else could — and a clear path to true healing."

Heather Bloom, MD, FACC, Director of Cardiac Electrophysiology, Atlanta VAMC Associate Professor, Emory University School of Medicine
"As a VA Electrophysiologist, I’ve used ANSAR’s Parasympathetic and Sympathetic Monitoring for years with outstanding results. It delivers diagnostic insights no other tool can provide. One case—a Navy SEAL suffering from severe dizziness and disability—was accurately diagnosed and effectively treated using ANSAR technology, after traditional tests failed. The patient regained his health, quality of life, and independence. This tool is a game-changer for patient care and healthcare efficiency."

Michael Stopyra, Patient
"I cannot say enough good things about Physio PS! This technology has done so much for me. I used to have terrible anxiety storms that would cause me to have high fevers. With this simple test, my doctor was able to find the root cause of my symptoms and prescribe a very low-dose medicine for about nine months to correct the primary problem. I have not had a high fever in four years!"

Copyright 2026. Physio PS, Inc.. All Rights Reserved.
The material and information provided by Physio PS is for general information purposes only. You should not rely upon this material or information for basis of making healthcare, treatment, or diagnosis decisions. While Physio PS strives to provide the most correct and up-to-date information and data, Physio PS makes no representations or warranties of any kind, expressed or implied, about the completeness, accuracy, reliability, suitability, or availability with respect to the information, products, services, or related graphics contained. Any reliance placed on such material is therefore strictly at your own risk. Reporting Information is supplied under license by NCRC LLC. * ‘RFa’ is known to be a measure of Parasympathetic activity and ‘LFa’ is known to be a measure of Sympathetic activity, based on reference: Colombo J, Arora RR, DePace NL, Vinik AI, Clinical Autonomic Dysfunction: Measurement, Indications, Therapies, and Outcomes. Springer Science + Business Media, New York, NY; 2014.


Facebook
Instagram
X
LinkedIn
Youtube